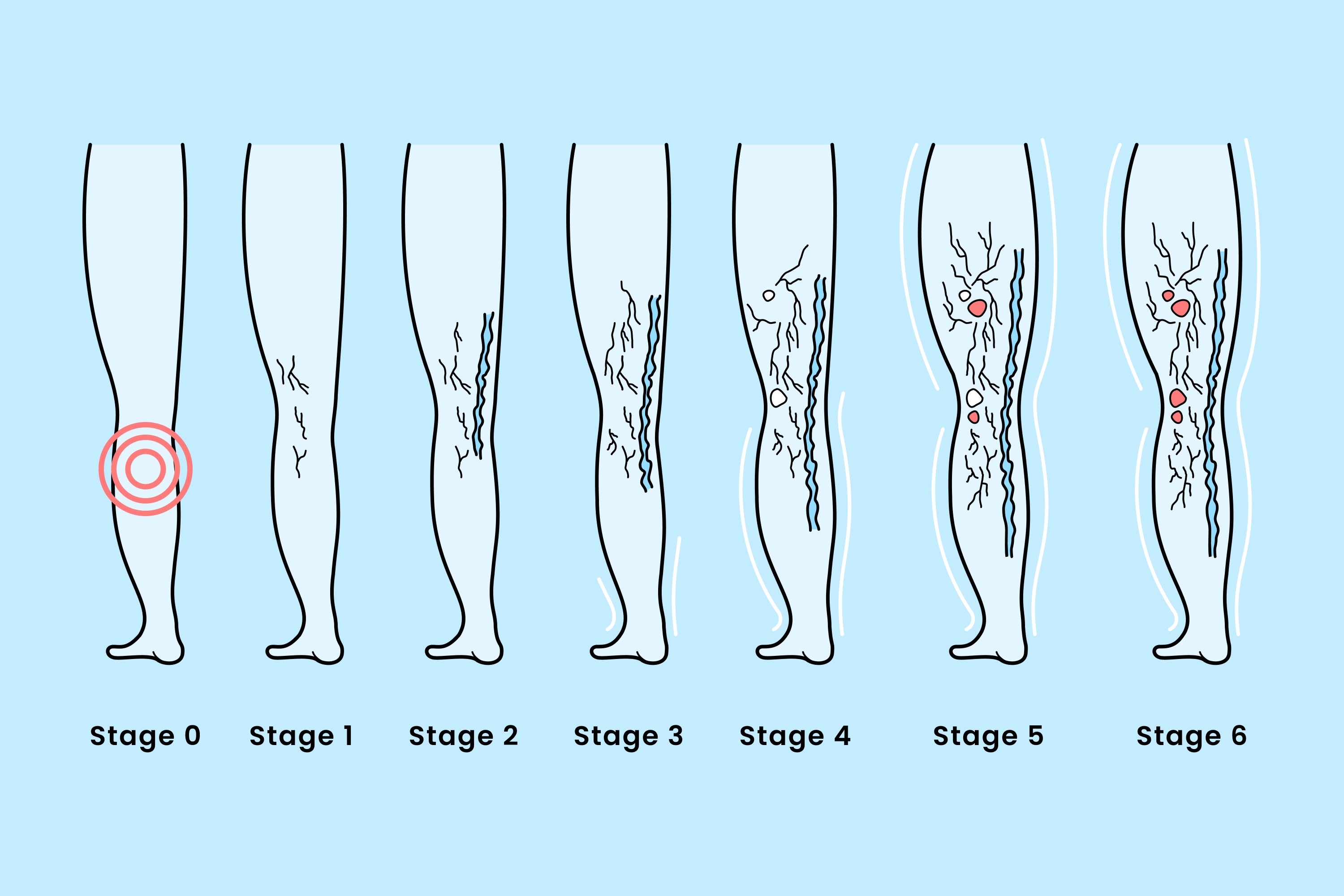
Varicose veins is a condition that affects a significant portion of the population, and its progression can lead to increasingly severe symptoms and complications. Understanding the clinical stages of varicose veins, as defined by the CEAP (Clinical, Etiology, Anatomy, Pathophysiology) classification system, is central to the effective management and treatment of varicose veins.
From early spider veins to advanced venous ulcers, the CEAP classification system provides a standardized framework for understanding varicose vein development.
Stage 0: Asymptomatic Preclinical Phase
Stage 0 is the preclinical stage, which involves early vascular changes without any visible symptoms. Risk factors for progressive vein disease, even in its early phases, include a genetic predisposition, family history, and lifestyle factors.
Vein changes in this stage will manifest as microscopic changes in vein walls and valves. Preventative measures include making lifestyle modifications, getting regular exercise, and maintaining a healthy weight.
Screening Recommendations: Regular check-ups for high-risk individuals.

Stage 1: Telangiectasias and Reticular Veins
This stage involves the appearance of telangiectasias and reticular veins.
- Telangiectasias (spider veins) are small, broken blood vessels that appear on the skin's surface.
- Reticular veins are visible veins (usually blue or purple) below your skin's surface that don't usually bulge.
A vein specialist can perform a vein health evaluation to differentiate Stage 1 symptoms from larger varicose veins.
Early intervention Strategies: May include sclerotherapy for cosmetic and symptom relief, addressing both aesthetic and medical concerns.
Stage 2: Visible Varicose Veins Without Symptoms
This stage presents with visible varicose veins but without any significant symptoms. Considered "uncomplicated" varicose veins, characteristics include visibly enlarged, twisted veins on the legs.
Primary vs. Secondary Varicose Veins
Primary varicose veins are caused by an anatomical weakness in the vein walls, often genetic, while secondary varicose veins are the result of underlying medical conditions like deep vein thrombosis (DVT), an obstruction, or injury.
Monitoring Strategies: Regular check-ups to track progression.

Stage 3: Varicose Veins With Symptoms
Stage 3 involves varicose veins accompanied by symptoms like aching, heaviness, fatigue, and swelling. Larger veins often correlate with more severe symptoms. Nighttime symptoms include nocturnal cramps and restlessness.
Those in this stage may experience a negative impact on their quality of life from reduced mobility and daily activity.
Symptom Assessment Tools: The Revised Venous Clinical Severity Score (VCSS) and other tools to quantify symptom severity.
Stage 4: Skin Changes Without Ulceration
Those in Stage 4 experience observable skin changes due to chronic venous insufficiency. These changes may include:
- Pigmentation Changes: Hemosiderin deposition and skin discoloration.
- Venous Eczema: Itchy, inflamed skin due to venous stasis (slow blood flow).
- Lipodermatosclerosis: Hardening and thickening of the skin.
- Atrophie Blanche: White, atrophic patches on the skin.
- Addressing Skin Complications: Topical treatments and compression therapy.
Stage 5: Healed Venous Ulcers
Stage 5 involves healed venous ulcers with a risk of recurrence. Healed ulcer sites show characteristics of previously ulcerated skin. The risk of recurrence is influenced by factors like poor circulation and delays in treatment. Ongoing compression therapy, leg elevation, and proactive skin care can help maintain the healing stage.
Preventative Strategies: Lifestyle modifications like exercising, maintaining a healthy weight, and scheduling regular check-ups.
Stage 6: Active Venous Ulceration
This stage involves active, open venous ulcers. Characteristics of active venous ulcers include symptoms like an open wound or visible sore and signs of infection like fluid or pus. Ulcers are diagnosed via a physical exam, a Doppler ultrasound, and laboratory testing, when necessary to rule out other conditions.
Venous vs. Arterial Ulcers
Venous ulcers are skin ulcers that develop when increased pressure causes vein valve failure and blood to flow in the reverse direction.
Arterial ulcers are caused when inadequate blood flows to the tissue, usually due to peripheral arterial disease.
Treatment Options
According to the Journal of Clinical Medicine, venous ulcers usually heal within six months with proper treatment.
Strategies to manage active ulcers include wound care protocols and compression, medications to treat pain and prevent infection, and sometimes advanced therapies, like skin grafts.
Progression Risk Factors
Certain lifestyle factors can accelerate the progression of varicose veins. These include:
- Smoking
- Obesity
- Age
- Prolonged standing or sitting
- Pregnancy and hormonal changes
Preventing Progression Between Stages
Lifestyle modifications and early interventions can prevent the progression of varicose veins. Exercise, elevating the legs, and the use of graduated compression can all slow down or even stop the worsening of varicose vein symptoms. Maintaining a healthy diet and weight can also be beneficial to your overall vein health.

When to Seek Medical Care
Some of the stage-specific warning signs to look for are pain, swelling, skin changes, and ulcers. Any worsening of varicose vein-related symptoms is cause for seeking medical care from a board-certified vein specialist.
Your vein care center can recommend the appropriate treatment for your varicose vein stage and help you access your insurance coverage for recommended treatments.
Conclusion
Appropriate staging for varicose veins is an important diagnostic tool for managing the progression of this common condition. A comprehensive approach, including lifestyle changes and medical interventions, can significantly improve long-term outcomes and your quality of life.
Discuss any new or worsening symptoms with your vein specialist, as early intervention in the early stages of varicose veins can prevent complications and unnecessary discomfort.
If you have noticed varicose veins on your legs or are having progressive symptoms in any stage, don't wait--book a free vein health evaluation at one of our convenient clinics.
Frequently Asked Questions
How quickly do untreated varicose veins typically progress from CEAP Class 2 to Class 4 with skin changes?
Progression varies, but skin changes can occur within a few years if left untreated.
What percentage of patients with Stage 3 varicose veins will eventually develop venous ulcers without intervention?
Approximately 5% of patients with Stage 3 will develop ulcers over time.
Can venous insufficiency return to Stage 1 from Stage 4 with proper treatment, or is skin damage permanent?
Skin damage can be permanent, but proper treatment can prevent further progression and improve symptoms.
How do diagnostic and treatment protocols differ between CEAP Classification Stage 2 versus Stage 5 varicose veins?
Stage 2 involves monitoring and lifestyle changes, while Stage 5 requires advanced wound care and interventions.
What objective measurements are used to determine transition between different CEAP stages of venous disease?
Diagnostic tools include Doppler ultrasound, VCSS, and skin assessments to track progression.

Dr. Jason Cumbers
Meet Dr. Jason Cumbers, MD, FACS, DABVS, RPVI, a highly-rated doctor specializing in the treatment of vein conditions. Schedule an appointment in NY today.
Meet Dr. Jason Cumbers
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.