Leg pain and swelling can impact your comfort and mobility, and could be signs of varicose veins. If you are experiencing these symptoms you may be wondering if it's simply visible varicose veins, or is something more complex going on? Getting an accurate diagnosis is the first step towards finding relief and getting back to feeling your best. Let's explore the various reasons behind leg pain and swelling and how to differentiate between them.
Understanding Varicose Veins
Varicose veins are large, distended veins that can develop as a result of poor blood flow in the legs. They often become visible on the legs and feet, look blue or purple, and commonly have a raised, rope-like appearance.
Common Symptoms of Varicose Veins
- A burning or throbbing discomfort, accompanied by leg cramps and swollen legs or ankles.
- A heavy or achy sensation in your legs
- Increased pain after prolonged periods of standing or sitting
- Itching around the affected veins
- Changes in skin color near the varicose veins
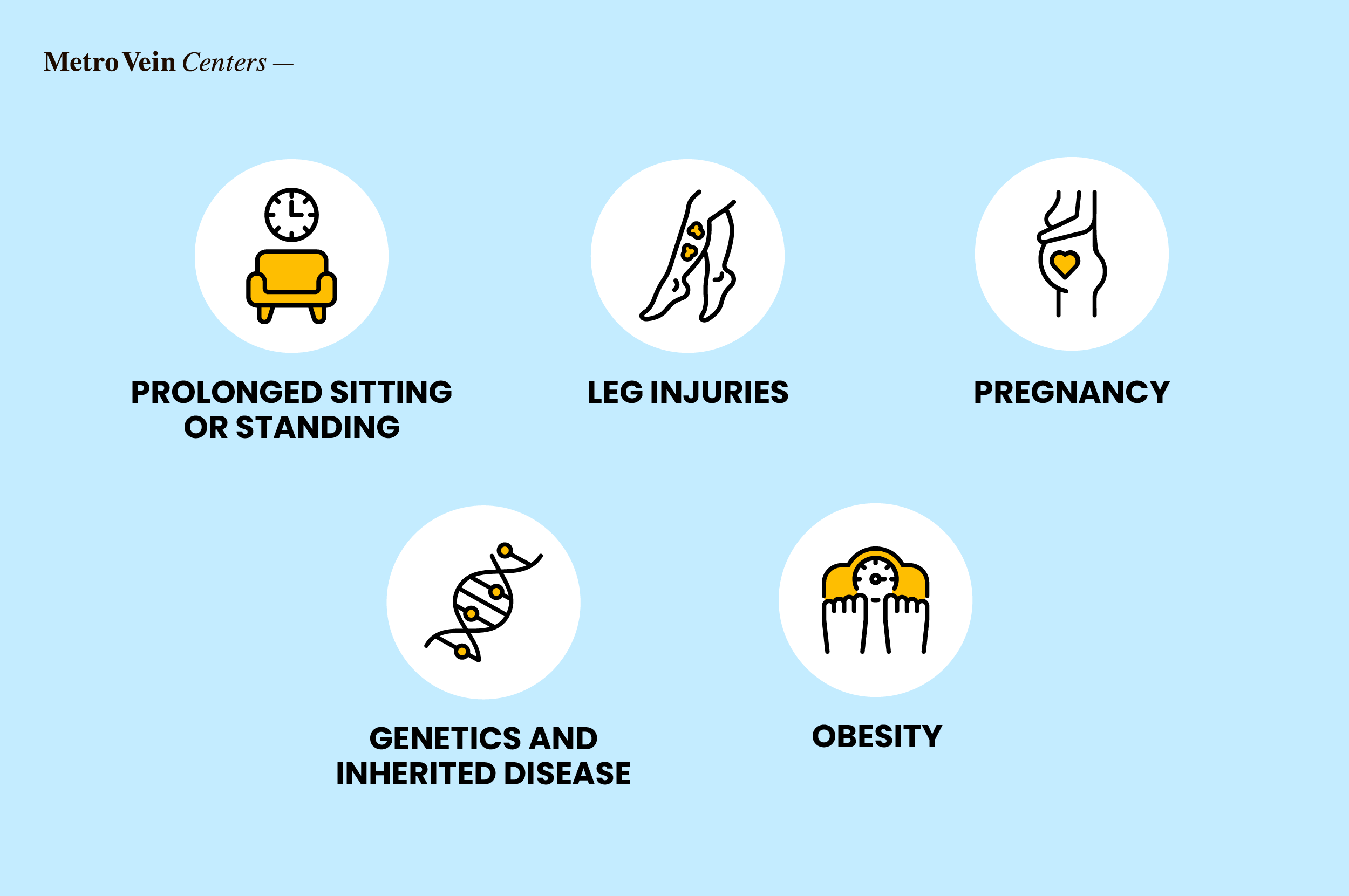
Causes of Varicose Veins
Varicose veins develop when the valves within your veins weaken, hindering the efficient return of blood to your heart. This leads to blood pooling in your legs, resulting in swelling and discomfort. Common causes of varicose veins include:
- Prolonged sitting or standing
- Leg injuries
- Pregnancy
- Genetics and Inherited disease
- Obesity
Other Potential Causes of Leg Pain and Swelling
While varicose veins are a frequent source of leg discomfort, other conditions can also contribute to leg pain and swelling:
Chronic Venous Insufficiency (CVI)
CVI is a term that encompasses vein circulation issues and is also known as vein disease. CVI occurs when your veins aren't able to pump blood back to your heart efficiently. This can lead to conditions like varicose and spider veins. Symptoms include leg swelling, pain, skin discoloration, and leg ulcers.
Deep Vein Thrombosis (DVT)
DVT is a serious condition involving a blood clot forming deep within your leg, causing significant pain, swelling, and redness.
Systemic Edema
Edema, also known as swelling, can also indicate underlying issues with your heart, kidneys, or liver, where fluid accumulates in your legs due to organ dysfunction.
Lymphedema
Leg swelling can also be caused by a condition called lymphedema. Lymphedema can develop as a result of a fluid build up due to an obstruction or when the lymphatic system becomes overwhelmed. Lymphedema can also cause swelling in the arms and other parts of the body.
Physical Injuries
Leg pain and swelling can also be caused by a physical injury or disease. These include muscle injuries/tears, sprains and broken bones, and arthritis.

Risk Factors of Leg Pain and Swelling
Understanding your risk factors can help you assess your likelihood of developing a condition that can lead to leg pain, swelling, and vein disease.
Varicose Veins
A family history of vein disease, being of advanced age, carrying excess weight, and prolonged periods of standing or sitting are all risk factors associated with varicose veins.
DVT
Risk factors for DVT include extended periods of inactivity, a recent surgery, smoking, and certain medical conditions.
Systemic Edema
Heart-related issues, kidney problems, and liver disease are associated with a higher risk of leg pain and swelling.
Lymphedema
Risk factors for lymphedema include genetics, injury, surgery, cancer, cancer treatment, and parasitic infection.
The Diagnostic Process
If you're experiencing persistent leg pain and swelling, your vein doctor or healthcare provider will likely:
Conduct a thorough medical history review: Discussing your symptoms, risk factors, and existing medical conditions.
Perform a physical examination: A vein evaluation can assess your legs for visible varicose veins, swelling, and skin changes.
Recommend diagnostic tests:
- Ultrasound imaging: To visualize blood flow in your veins.
- Doppler studies: To measure blood flow in your arteries and veins.
- Blood tests: To rule out other potential causes, such as DVT or systemic issues.
Navigating Treatment Options
Treatment approaches will vary depending on the underlying cause of your leg pain or swelling. Treatments for the medical conditions listed below may include:
Varicose Veins
- Compression therapy/garments
- Regular exercise and weight management
- Sclerotherapy (injecting a sclerosing agent to close the vein)
- Radiofrequency ablation (using heat to seal the vein)
DVT
- Anticoagulant medications (blood thinners)
Systemic Edema
- A referral to your primary care physician
- Diuretic medications (water pills)
- Proactive prevention and lifestyle adjustments

Urgent Warning Signs
These are some of the signs that your leg pain and swelling has graduated to an urgent medical event necessitating immediate medical attention:
- Sudden, intense leg pain coupled with swelling
- Chest discomfort or shortness of breath (a possible DVT complication)
- Skin ulcers, bleeding, or open wounds
- Rapidly increasing swelling
Strategies to Promote Leg Health
Taking proactive measures can go a long way in preventing leg discomfort, swelling, and the worsening of vein disease. Here are some effective strategies to promote healthy circulation and keep your legs in top shape.
- Engage in regular physical activity to enhance circulation.
- Maintain a healthy weight to reduce pressure on your veins.
- Elevate your legs to minimize swelling.
- Wear compression stockings to support your veins and improve blood flow.
- Avoid prolonged periods of sitting or standing; take frequent breaks to move around.
Key Takeaways
Leg pain and swelling can stem from various causes, ranging from varicose veins to more serious conditions like DVT. Getting an accurate diagnosis from a vein specialist is essential for effective management. Remember, early intervention and a proactive approach can significantly improve your vascular health.
Are you experiencing leg pain or swelling? Schedule an appointment with our vein specialists today for a free, personalized evaluation and a tailored treatment plan.
Frequently Asked Questions
How can I differentiate between leg swelling caused by varicose veins and other conditions?
Watch for urgent symptoms such as sudden, severe pain, redness, or chest pain, which may indicate DVT or another serious condition.
What diagnostic tests are used to distinguish varicose veins from other conditions like DVT or edema?
At an appointment with a vein specialist, your doctor may use diagnostic tests to diagnose vein disease such as ultrasound, Doppler studies, and blood tests.
Can lifestyle modifications effectively alleviate leg pain and swelling?
Regular exercise, weight management, and leg elevation may help manage these symptoms.
When should I seek medical attention for persistent leg pain?
If your symptoms don't improve or worsen or if they are accompanied by shortness of breath or chest pain then you should seek immediate medical attention.
What treatment options are available if my leg pain is not attributed to varicose veins?
The treatment option would be dependent on the cause of the leg pain. For example, if the pain was caused by a DVT, anticoagulant therapy would be the treatment of choice.
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.






